Type 1 diabetes (T1D) is caused by the autoimmune destruction of insulin-producing beta cells in the pancreas. People with T1D are dependent on insulin therapy to control their blood sugar levels, which is critical to prevent complications that occur when blood sugar is too high (hyperglycemia) or too low (hypoglycemia).
The best bet for T1D cures depends on cell therapies, which replace destroyed beta cells with protected, functional cells to restore insulin therapy independence and glucose control, ideally without chronic immunosuppression. Breakthrough T1D’s Cures Program has been instrumental in the incredible progress we’ve made in cell therapies research. The secret to success? Stem cells.
What are stem cells?
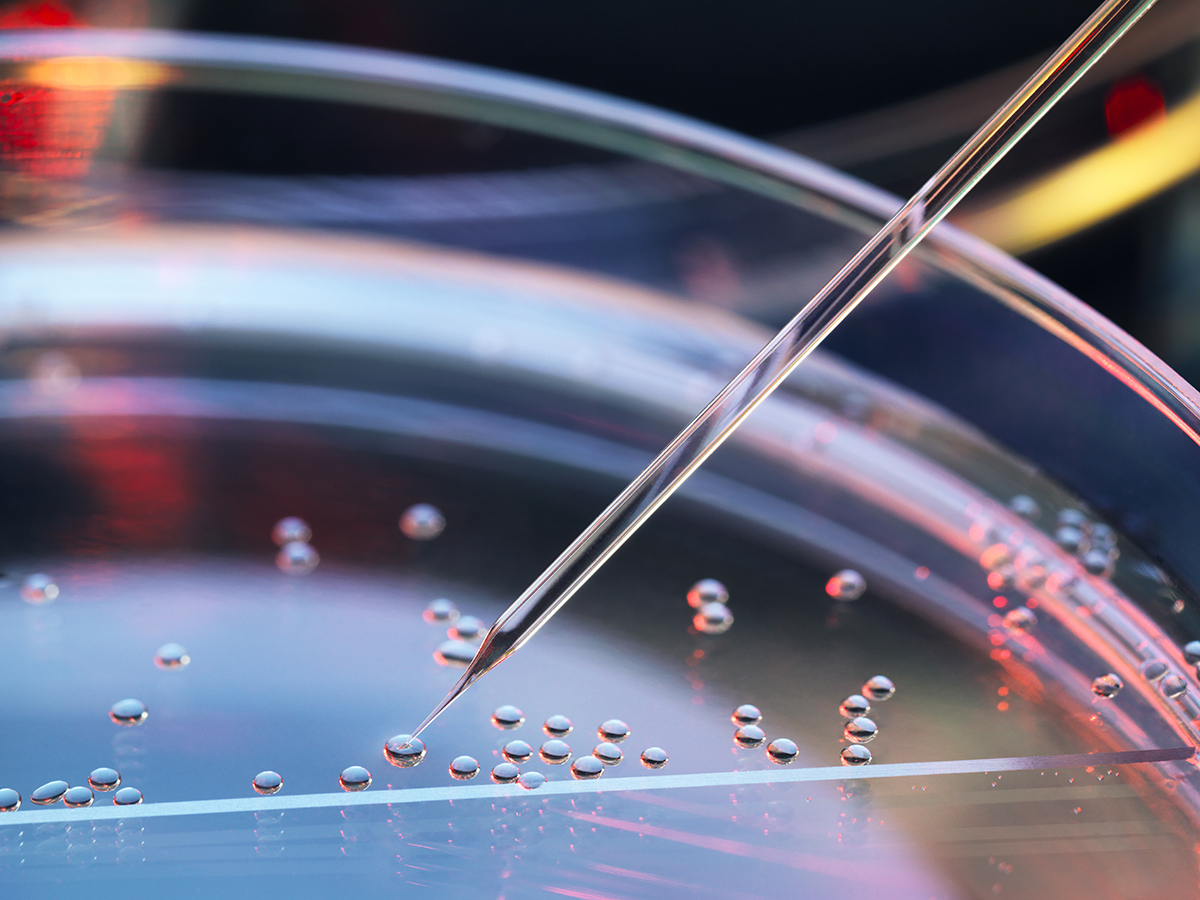
Stem cells are uniquely suited for use in cell therapies because of their biological characteristics. First, they are essentially a blank slate—we can biologically engineer them to become any cell we want, including beta cells. Second, stem cells can make copies of themselves while remaining a blank slate, meaning we can generate an unlimited source of transformable cells.
Since scientists first isolated human stem cells in 1998, there has been major progress in therapies that can replace or renew damaged and diseased tissue. For example, people with blood cancer often undergo chemotherapy and radiation to destroy cancerous blood cells. Stem cells are delivered directly into the bloodstream and travel to the bone marrow, where they transform into new, non-cancerous blood cells, replacing the important cells that were lost with healthy ones. The exciting progress in stem cell research extends to T1D—researchers have harnessed the power of stem cells to generate functional beta cells and islets, rapidly accelerating the drive toward T1D cures. Breakthrough T1D has been at the forefront of stem cell research in T1D for decades.
Stem cells are the foundation of our Cell Therapies Program
Breakthrough T1D’s Cell Therapies Program focuses solely on making and improving stem cell-derived beta cells. For stem cell-based therapies to become a reality for everyone with T1D, there are three primary goals that we are striving to achieve:
- First, we need to generate a renewable, scalable source of beta cells so that there are enough for everyone who needs them.
- Second, we need to find a habitable site to implant beta cells so that they remain functional and healthy for very long periods of time.
- Third, we must find a way to protect implanted beta cells from immune attack so that people won’t need to take chronic anti-rejection immunosuppressants, which can come with intolerable side effects.
Breakthrough T1D has put tremendous effort into achieving these goals; we’ve seen incredible progress in recent years, pushing us closer than ever to cures for T1D.
Breakthrough T1D has driven more than $156 million to cell therapies research in the past decade and has spearheaded several initiatives to drive this effort forward. In 2013, the Beta Cell Replacement Consortium was launched, bringing together 50+ of the brightest scientists and key industry players to integrate expertise in bioengineering, animal models, transplant medicine, and other key research areas.
Similarly, Breakthrough T1D established several Centers of Excellence, a collection of institutions driving exceptional advancements in immunology, stem cell biology, and gene editing, all of which are critically important to cell therapies research. The ultimate goal of these initiatives is to foster collaboration, exchange resources and data, and accelerate the development of stem cell-derived islet therapies.
Project ACT
To further support these efforts, Breakthrough T1D most recently launched Project Accelerate Cell Therapies (Project ACT) to simultaneously push research, development, regulatory policies, access, and adoption to increase the rate at which cell therapies without the need for broad immunosuppression will become available to people with T1D. This is important because, at this time, cell therapies require anti-rejection immunosuppressants, which can come with serious long-term side effects that may not be tolerable for everyone with T1D.
Looking forward
With Breakthrough T1D’s commitment to driving cell therapies forward, we have made significant headway in the development of life-changing therapies that can place healthy, insulin-producing beta cells back into people with T1D. “Even with today’s fantastic automated insulin delivery systems and advanced algorithms, those living with T1D still spend a significant amount of time interacting with their devices in order to maintain blood sugar control,” said Nicholas Mamrak, a scientist at Breakthrough T1D. “The prospect of cell therapies lies in the ability to take off these pumps and spend less time managing and worrying about their diabetes.”
The drive toward stem cell-based therapies becoming a reality for everyone with T1D continues—despite how far we’ve come, we still have more work to do.
This article is the first of a three-part series exploring the significance of stem cells in cell replacement therapies for T1D. Stay tuned for the next article, which will dive deeper into the history of stem cell research and T1D.