In honor of the 100th anniversary of the first administration of insulin, Breakthrough T1D launched “100 Years, 100 Breakthrough T1D Scientists,” to tell the story of scientists and their discoveries, which put together the vast knowledge that we have about diabetes today.
The next one, for Healthy Vision Month: Treatments for diabetic eye disease.
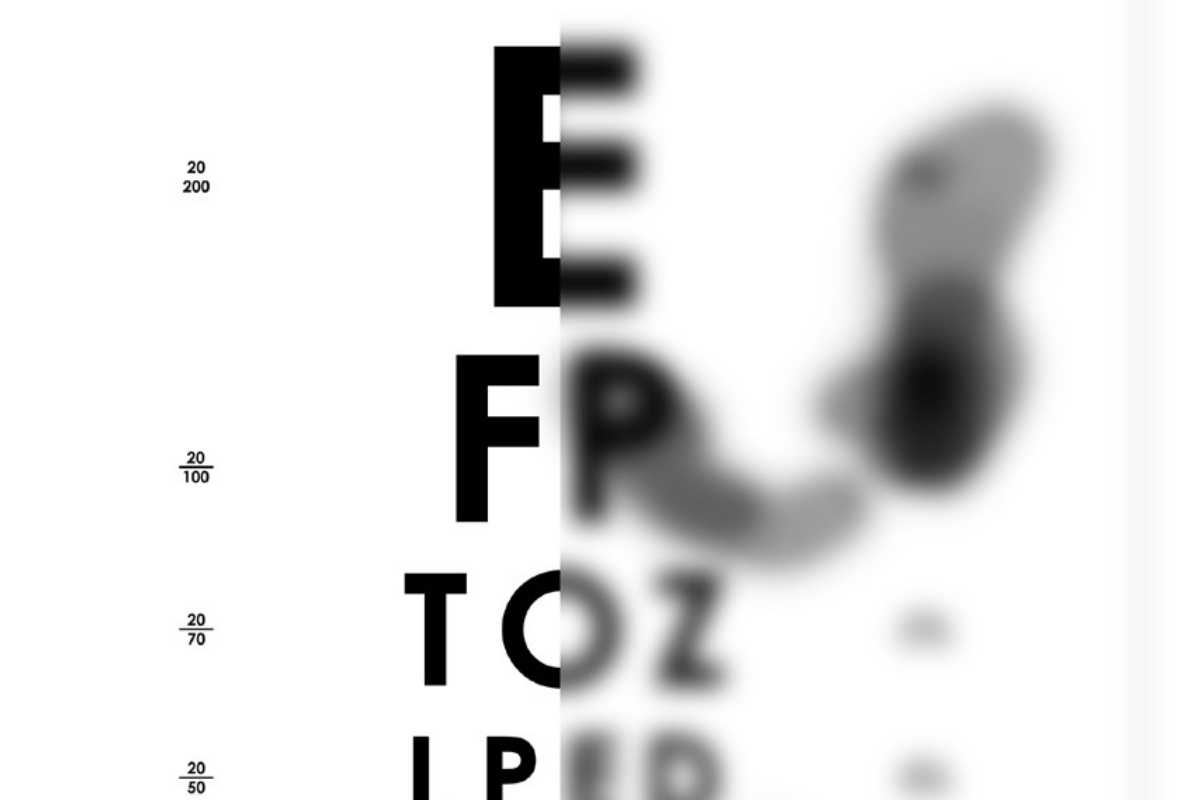
Several decades ago, blindness and severe vision loss occurred in 40 percent of people with diabetes, but we have made progress since that time. Early detection and timely, appropriate treatment can reduce the risk of blindness by over 95 percent. Nonetheless, tens of millions of people, worldwide, still suffer from limited vision and blindness due to diabetes and the side effects of current treatment methods, and there is a real need to redouble our efforts to develop advanced and effective new therapies to restore vision and “cure” blindness in those so affected and prevent visual loss in the first place in people at risk.
The retina is a thin layer of specialized nerve tissue on the back wall of the eye. It converts light into electric signals that are transmitted to the brain where the images we “see” are generated. The center of the retina, called the macula, is responsible for the sharp clear vision needed for reading and other daily tasks. Abnormal leaking from blood vessels damaged by diabetes can lead to swelling of the macula and vision loss. Diabetes also causes direct damage to nerve cells of the eye, including cells in the periphery of the retina. These changes stimulate the development of abnormal blood vessels, which are fragile and can bleed and further destroy the nerve tissue around them, scarring the retina and putting people at high risk for low vision and blindness.
Starting in the 1970s and 1980s, Breakthrough T1D supported the pioneering work of Lloyd M. Aiello, M.D., who, along with William P. Beetham, M.D., was a pioneer in introducing retinal photocoagulation therapy—a laser treatment that intentionally scars the peripheral retina in an effort to preserve the central vision needed for reading. Laser therapy has been successful in reducing the rate of blindness and severe central visual loss in proliferative retinopathy, as well as reducing progression of diabetic macular edema.
In the 1990s, Breakthrough T1D supported multiple research grants, including one proposed by Lloyd Paul Aiello, M.D., Ph.D. (Lloyd M.’s son), and George King, M.D., that showed that levels of VEGF, a protein the body makes which promotes the growth of new blood vessels in the eye, were elevated in people with diabetic retinopathy. Blocking VEGF substantially reduced the development of these fragile, leaky new blood vessels, suggesting that inhibiting VEGF might be a potential treatment for diabetic retinal disease.
For their contributions to research, Dr. Lloyd M. Aiello, Lloyd P. Aiello, and George King received prestigious Breakthrough T1D awards; the former two were given the prestigious David Rumbough Awards, and the latter was given the Breakthrough T1D Mary Tyler Moore and S. Robert Levine, MD Award for Excellence in Clinical Research.
Clinical Development and Regulatory Approval
Lucentis® (ranibizumab) and Eylea® (aflibercept), which are designed to inhibit VEGF, are two approved therapies for diabetic macular edema and diabetic retinopathy. Lucentis was approved in August 2012, and Eylea was approved in March 2015.
Breakthrough T1D played a critical part in clinical studies that led to their approval. A clinical trial of Lucentis (ranibizumab), funded by Breakthrough T1D and run by Quan Dong Nguyen, M.D., and Peter Campochiaro, M.D., demonstrated that this is an effective treatment for diabetic macular edema, with eyesight improving significantly for the 10 patients tested. They would go on to complete two clinical trials—READ 2 and READ 3—that showed substantial improvement in eyesight in people with diabetic macular edema treated with the drug.
In 2013, an estimated 90 percent of retinal specialists in the United States reported treating vision loss from diabetic macular edema with anti-VEGF therapy.
Through the Restoring Vision Moonshot, a special initiative of the Mary Tyler Moore and S. Robert Levine Charitable Foundation and Breakthrough T1D launched to honor Mary’s contributions to diabetes awareness and research, Breakthrough T1D is now supporting additional research to find new ways to prevent the development of diabetic retinal disease, arrest its progression to preserve visual function, and restore lost vision.
Ensuring eye complications research continues, and accelerating the finding of “cures” for low vision and blindness and preventive treatments for diabetic retinal disease is extremely important to Breakthrough T1D and our T1D community.